
Ethylene Oxide (EtO) gas is one of the most common ways to sterilize medical devices, a safe, tightly controlled, highly regulated process which is critical for preventing infections and ensuring patients have safe surgeries and medical treatments.
Ethylene oxide (EtO) is a versatile compound used in a variety of industrial applications and everyday consumer products, personal care items, as well as fabrics and textiles.
A small but critically important use of ethylene oxide is the sterilization of medical devices, including the sterilization of personal protective equipment used by doctors and hospitals across the country in the fight against the COVID-19 pandemic.
It is estimated that ethylene oxide sterilizes 20 billion medical devices each year, helping to prevent disease and infection. According to the FDA, this represents more than half of sterilized medical supplies in the United States, making EtO a key component in the nation’s healthcare industry supply chain.
For many medical devices, due to their size, shape, complexity or material composition, EtO is the only option for sterilization. For these products, alternatives such as steam, radiation or other sterilants do not achieve the needed levels of sterility assurance. In addition, for some medical devices, using non-EtO sterilization methods will result in material degradation, rendering the products potentially unsafe for patients.
“What Laredo Needs to Know About Ethylene Oxide” in the Laredo Morning Times by Terry Chang of AdvaMed
“[T]here is no cancer threat from the tiny amounts of ethylene oxide released from these sterilization plants.”
—Gail Charnley, PhD, Senior Toxicologist, HealthRisk Strategies LLC
“To be clear – there are no actual scientific data that show that these [EtO] exposure levels result in cancer.”
—Lucy H. Fraiser, board-certified toxicologist (Diplomate of the American Board of Toxicology)
“Ethylene oxide has been, and is, extensively regulated. The rules that EPA first put into place to establish ethylene-oxide sterilization procedures were carefully designed and extremely stringent… As a result of these regulations, ethylene-oxide emissions remain incredibly low—far lower than a number of other potentially harmful HAPs, in fact.”
—Richard J. Trzupek, The Heartland Institute
“…Ethylene oxide is a commonly used method of medical device sterilization. It’s considered a safe and effective method that helps ensure the safety of medical devices and helps deliver quality patient care.”
—Dr. Scott Gottlieb, former FDA commissioner
“There are avenues that might lead to replace ethylene oxide, but the standards aren’t there yet. If we’re going to get rid of [EtO] it’s going to take 10-20 years.”
—Gary Secola, president, HIGHPOWER Validation Testing & Lab Services; member of FDA’s General Hospital and Personal Use Panel of the Medical Devices Advisory Committee
“If there’s an ubiquitous ban on ethylene oxide today, we’re going to have a health crisis on our hands, because in very short time and order, sterile products won’t be available, and we don’t have an alternative to replace that today.”
—Marcus Schabacker, MD, PhD, President and CEO, the ECRI Institute
“Currently, there are no validated industrial sterilisation alternatives that could completely replace EtO sterilisation, so additional closures of EtO processing facilities would have the potential to impair the U.S. healthcare system.”
—Dr. Amanda Sivek, principal project engineer, health devices, also of the ECRI Institute
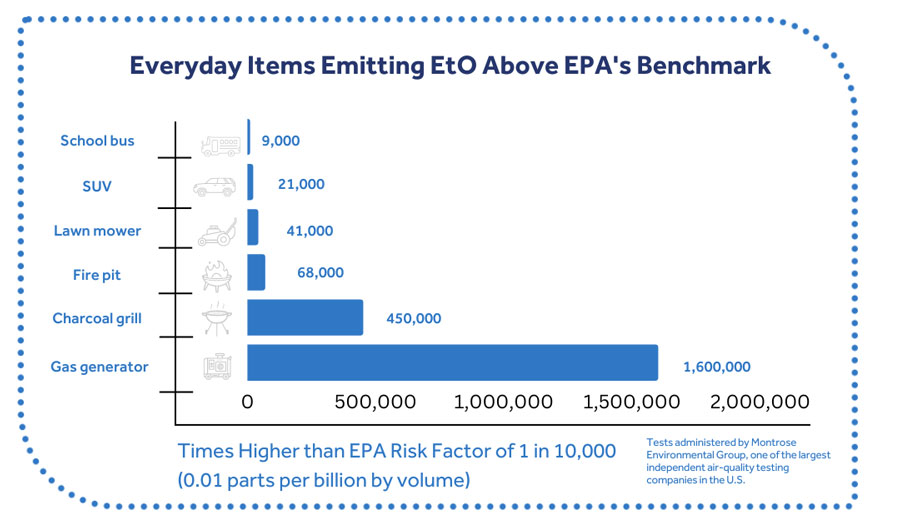
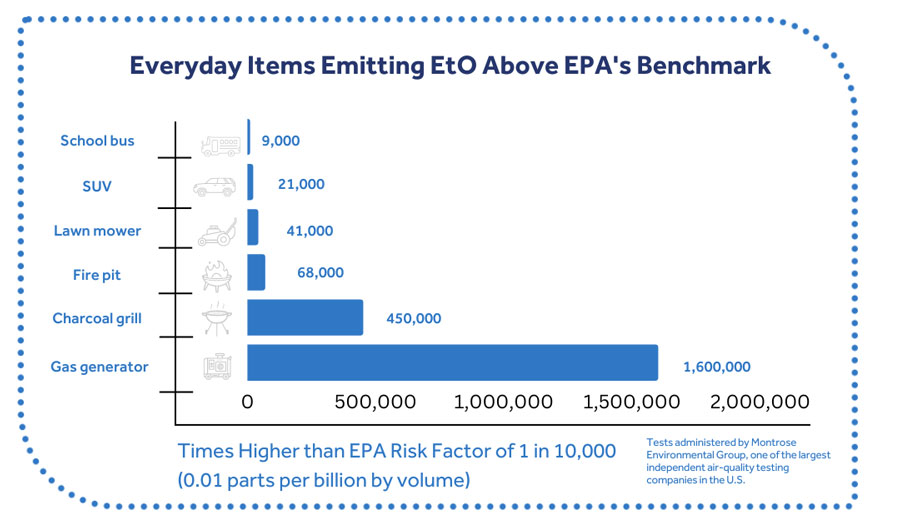
Ethylene oxide is naturally present in the environment and is created by various sources, including plants and animals. The human body also converts ethylene to ethylene oxide and emits it during respiration. Natural levels of ethylene oxide vary across urban, suburban and rural environments; and result in human exposure.
EtO sterilization is a highly regulated process, and device manufacturers, hospitals and third-party sterilizers must follow rigorous controls established by EPA, OSHA and other government agencies (including state and local entities) to protect patients, workers and the environment.
While EtO is a recognized hazardous chemical, federal regulations and international guidance on emissions, residuals and worker safety allow for the safe and responsible use of EtO to sterilize medical products. Device manufacturers and sterilizers responsibly capture, remove, and destroy EtO with the best available technologies on the market today.
In many instances, companies exceed current mandates of 99% destruction; often achieving levels of 99.9% and higher. Industry continues to improve its application of abatement technologies and employs continuous improvement activities as appropriate.
A 2014 National Air Toxics Assessment (NATA) by the EPA used a flawed risk value for ethylene oxide that is not based on the best available science. The risk value was generated by EPA’s Risk Information System (IRIS) program, which neglected to consider certain comprehensive, highly relevant studies.
The risk value is far below levels found in nature. Is it 19,000 times lower than the naturally-created levels of EtO in the human body and is far lower than the concentrations found in ambient air in states where there are no EtO production or sterilization facilities.
AdvaMed, the National Academies of Sciences, U.S. Government Accountability Office, Congress, state environmental authorities, and many in the scientific community—including two EPA Science Advisory Boards—have found serious, longstanding problems with the IRI EtO assessment.
Nonetheless, this flawed science has been used by activists as the basis for a misguided campaign seeking to stop EtO use—which directly compromises the nation’s ability to sterilize critical medical equipment. Sound science should always inform our public health decisions. However, the flawed IRIS assessment is being politized to create a needless public health crisis.
EtO sterilization facilities are not only required to install emission control technologies, but meet EPA standards such as continuous emissions monitoring, emission controls, performance testing, and mandated reporting and record keeping.
This is why we don’t have to rely on speculative assessments to determine whether or not EtO sterilization facilities currently pose a public health risk. There are continuous and up-to-date air quality monitoring reports that confirm – individuals and communities near EtO sterilization facilities are not exposed to any higher levels of EtO than anywhere in the country.
For example, areas in the state of Georgia are being monitored by state and federal authorities as part of continued efforts to qualify EtO levels in the air. This has resulted in vast amounts of air monitoring data that provide insights to actual levels of ethylene oxide (EtO) present in greater Atlanta and across Georgia.
As of Aug. 20, 2020, the Georgia Environmental Protection Division (EPD) released its latest EtO air monitoring data for a variety of areas around the state. This data shows that average levels of EtO in Covington, Ga. – where a sterilization facility exists – are exactly the same as the levels found in the rural General Coffee State Park and below levels found at EPD’s background monitoring station in South DeKalb, Ga. (approximately 30 miles from the Covington facility).
The data also reveals that average levels across the greater Atlanta area are about the same in areas where there are EtO sterilization facilities and areas where there are not. Consequently, the data suggests that those who live in communities with sterilization facilities are exposed to similar amounts of EtO as those who do not live near the facilities because of other sources of EtO, including naturally occurring sources.